Insight, into Diabetes
Diabetes is a health condition that affects individuals of all age groups with Type 2 being the common form. Successfully managing this condition involves a combination of therapies to maintain a quality of life and prevent health issues.
What is Diabetes?
Diabetes occurs when there is a level of glucose or sugar in the bloodstream. This can happen due to insulin production by the pancreas inadequate insulin response in the body or no insulin being produced at all. It can impact people regardless of their age. While many cases are chronic they can be controlled through medications and lifestyle modifications.
Glucose primarily comes from carbohydrates found in food and beverages serving as the body’s energy source. It travels through the bloodstream to nourish all cells for energy purposes. Insulin, acting like a “key” facilitates glucose entry into cells. In cases where the pancreas fails to produce insulin or if it is not effectively utilized by the body glucose accumulates in the blood leading to high blood sugar levels (hyperglycemia).
Elevated blood sugar levels over time can lead to health complications such, as heart disease, nerve damage and vision problems. The term used to describe this condition is diabetes.
It’s important to note that there exists another condition known as diabetes insipidus, which despite sharing a name and some similar symptoms, like thirst and frequent urination is less common and distinct from diabetes mellitus.
Exploring Different Types of Diabetes
Diabetes manifests in forms with the following being the most familiar;
- Type 2 Diabetes; This type occurs when the body either doesn’t produce insulin or the cells become resistant to its effects (referred to as insulin resistance). It is commonly observed in adults. Can also affect children.
- Prediabetes; Regarded as a precursor to Type 2 diabetes prediabetes involves blood sugar levels that are higher than normal but not at a level for a Type 2 diabetes diagnosis.
- Type 1 Diabetes; This autoimmune condition involves the immune system mistakenly attacking and destroying insulin-producing cells in the pancreas. While it can occur at any age it is usually diagnosed in children and young adults accounting for 10% of all diabetes cases.
- Gestational Diabetes; This form occurs during pregnancy. Typically resolves after giving birth. However, individuals with diabetes are, at risk of developing Type 2 diabetes.
Different types of diabetes include;
- Type 3c Diabetes; Occurs due, to damage to the pancreas not caused by known factors affecting its insulin production. Causes can include pancreatitis, pancreatic cancer, cystic fibrosis, hemochromatosis or post-surgery effects.
- Latent Autoimmune Diabetes in Adults (LADA); Resembles Type 1 diabetes but progresses gradually and is typically diagnosed in individuals over 30 years old.
- Maturity-onset Diabetes of the Young (MODY); Results from a mutation that causes inherited diabetes impacting insulin production and use. Various types of MODY affect around 5% of people with diabetes. Often run in families.
- Neonatal Diabetes; A condition affecting infants under six months old which can be either diabetes mellitus) or temporary (transient neonatal diabetes mellitus) with the latter potentially recurring later in life.
- Brittle Diabetes; This form of Type 1 diabetes is characterized by fluctuations, in blood sugar levels leading to hospitalizations. In some instances, a pancreas transplant may be considered as a long-term treatment option.
Is Diabetes Common?
Diabetes poses a health concern.
In the United States 37.3 million people, making up 11% of the population are dealing with diabetes. The vast majority of these cases around 90% to 95% are classified as Type 2 diabetes.
Looking at a scope there are 537 million adults worldwide living with diabetes. Estimates suggest that this number could rise to, about 643 million by 2030 and potentially reach, up to 783 million by the year 2045.
Diabetes Symptoms and Causes
The intensity of diabetes symptoms can differ depending on the diabetes type. Symptoms tend to be more pronounced in individuals with Type 1 diabetes compared to those with Type 2 diabetes.
Common Symptoms of Diabetes The signs of diabetes can include:
- Increased thirst (polydipsia) and a dry mouth.
- The need to urinate frequently.
- Persistent tiredness.
- Blurry vision.
- Unintended weight loss.
- Numbness or a tingling sensation in the hands or feet.
- Cuts or sores that heal slowly.
- Recurring skin and/or vaginal yeast infections.
If you or your child exhibits these symptoms, it’s crucial to consult a healthcare provider.
Symptoms Specific to Diabetes Types
- Type 1 Diabetes: Symptoms can emerge swiftly, within weeks or months, and may be accompanied by signs of a serious condition known as diabetic ketoacidosis (DKA), which is life-threatening and demands immediate medical attention. Symptoms of DKA include vomiting, abdominal pain, fruity-smelling breath, and laboured breathing.
- Type 2 Diabetes and Prediabetes: Often, there may be no noticeable symptoms, or they may appear gradually, making them hard to detect. High blood sugar levels might only be discovered through routine blood tests. A sign of prediabetes could be darkened areas of skin, known as acanthosis nigricans.
- Gestational Diabetes: Typically, gestational diabetes does not present noticeable symptoms. Healthcare providers screen for this condition between the 24th and 28th weeks of pregnancy.
Understanding the Causes of Diabetes
Diabetes is characterized by an excess of glucose in the bloodstream, which is a common factor across all types of the condition. However, the underlying reasons for elevated blood glucose levels vary by diabetes type.
Key Contributors to Diabetes
- Insulin Resistance: This is the primary cause of Type 2 diabetes. It occurs when muscle, fat, and liver cells do not respond adequately to insulin. Factors like obesity, sedentary lifestyle, dietary habits, hormonal changes, genetic predisposition, and certain medications can induce or exacerbate insulin resistance.
- Autoimmune Response: Both Type 1 diabetes and Latent Autoimmune Diabetes in Adults (LADA) are the result of the body’s immune system mistakenly attacking the insulin-producing beta cells in the pancreas.
- Hormonal Changes: Gestational diabetes arises when pregnancy hormones lead to insulin resistance, and the pancreas cannot compensate with enough insulin production. Other conditions, such as acromegaly and Cushing’s syndrome, can also induce insulin resistance, potentially leading to Type 2 diabetes.
- Pancreas Damage: Any damage to the pancreas from illness, surgical intervention, or physical injury can impair its insulin-producing capability, leading to Type 3c diabetes.
- Genetic Factors: Specific genetic mutations are responsible for causing Maturity Onset Diabetes of the Young (MODY) and neonatal diabetes.
Additionally, long-term usage of certain drugs, including those for HIV/AIDS and corticosteroids, may contribute to the development of Type 2 diabetes.
What are the Complications Associated with Diabetes?
Diabetes, characterized by consistently high levels of blood sugar, can precipitate both immediate, severe complications and chronic health issues over time.
What are the Immediate Risks of Diabetes?
Some of the life-threatening immediate complications include:
- Hyperosmolar Hyperglycemic State (HHS): Predominantly seen in individuals with Type 2 diabetes, HHS is a condition resulting from extremely high blood sugar levels (above 600 mg/dL) that persist, leading to significant dehydration and confusion. This condition demands urgent medical attention.
- Diabetic Ketoacidosis (DKA): This complication is more common among those with Type 1 diabetes or undiagnosed cases. It occurs when there’s insufficient insulin, prompting the body to break down fats for energy, producing ketones and acidifying the blood. Symptoms include difficulty breathing, vomiting, and unconsciousness, necessitating immediate medical care.
- Severe Hypoglycemia: A dangerously low blood sugar level, primarily affecting those who manage their diabetes with insulin. Symptoms include blurred or double vision, coordination problems, confusion, and seizures, requiring emergency treatment with glucagon or medical intervention.
What are the Chronic Complications of Diabetes?
Prolonged high blood sugar can inflict damage on various organs and tissues, especially the blood vessels and nerves, leading to:
- Cardiovascular complications such as coronary artery disease, heart attacks, strokes, and atherosclerosis.
- Nerve damage (neuropathy), manifesting as numbness, tingling, or pain.
- Kidney damage (nephropathy), potentially requiring dialysis or a kidney transplant.
- Eye damage (retinopathy), which can cause blindness.
- Foot problems due to nerve damage and poor blood flow, leading to infections and possibly amputations.
- Skin conditions, including infections.
- Sexual dysfunction, such as erectile dysfunction or vaginal dryness, stemming from nerve and blood vessel damage.
- Gastroparesis, a delay in stomach emptying.
- Hearing impairment.
- Dental issues like gum disease.
Moreover, diabetes can significantly impact mental health, increasing the risk of depression two to three times compared to individuals without diabetes.
Diagnosis and Testing for Diabetes
Identifying Diabetes
How do healthcare professionals diagnose diabetes?
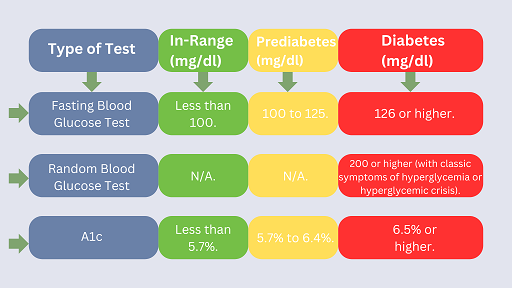
The diagnosis of diabetes is confirmed through blood tests that measure your glucose levels. There are three main types of tests used for this purpose:
- Fasting Blood Glucose Test: This requires fasting for at least eight hours before the test, with no food or drink consumed except water. This fasting helps to determine your baseline glucose level since food intake significantly influences blood sugar levels.
- Random Blood Glucose Test: This test can be performed at any time, regardless of when you last ate, making it a “random” measure of your blood sugar levels.
- A1c Test: Also known as the HbA1C or glycated haemoglobin test, this assesses your average blood sugar over the last two to three months.
For detecting gestational diabetes, an oral glucose tolerance test is administered.
Test results are used to categorize individuals as not having diabetes, having prediabetes, or having diabetes. These diagnostic thresholds can vary slightly. Furthermore, healthcare providers typically rely on multiple tests to ensure accuracy before making a diabetes diagnosis.
What are the Management and Treatment Strategies for Diabetes?
Handling Diabetes
What approaches are taken to manage diabetes?
The management of diabetes is multifaceted and tailored to each individual, as the condition manifests uniquely in each person. The management regimen encompasses several critical components:
- Monitoring Blood Sugar Levels: A cornerstone of diabetes management is the regular monitoring of blood sugar levels. This monitoring helps assess the effectiveness of your treatment plan, guiding daily and sometimes hourly management decisions. Blood sugar can be tracked through regular testing with a glucose meter and finger sticks or by using a continuous glucose monitor (CGM). The appropriate blood sugar targets are determined in partnership with your healthcare provider.
- Oral Medications: For those who still produce some insulin, particularly individuals with Type 2 diabetes and prediabetes, oral medications play a significant role in managing blood sugar levels. This also applies to some cases of gestational diabetes. Metformin is among the most commonly prescribed oral medications.
- Insulin Therapy: Synthetic insulin injections are essential for individuals with Type 1 diabetes and some with Type 2 diabetes to manage their condition. Various types of insulin are available, differing in how quickly they act and how long their effects last. Insulin can be administered via syringes (injections), insulin pens, insulin pumps, or rapid-acting inhaled forms.
- Dietary Management: Proper nutrition and meal planning are vital, as what you eat significantly affects blood sugar levels. For those on insulin, carbohydrate counting is crucial to determine the necessary insulin dose per meal. Adopting healthy eating habits can also support weight management and reduce the risk of heart disease.
- Physical Activity: Regular exercise enhances insulin sensitivity, making it a key element of diabetes management for all patients. This helps in mitigating insulin resistance.
Additionally, managing diabetes effectively also means maintaining a healthy weight, keeping blood pressure in check, and managing cholesterol levels, due to the heightened risk of heart disease associated with diabetes.
Preventing Diabetes
What steps can be taken to reduce the risk of diabetes?
While it’s not possible to prevent all forms of diabetes, especially those due to autoimmune issues and genetics, you can take measures to lower your risk of developing prediabetes, Type 2 diabetes, and gestational diabetes. These steps include:
- Adopting a nutritious diet, like the Mediterranean diet.
- Engaging in physical activity, aiming for at least 30 minutes on most days of the week.
- Striving for and maintaining a healthy weight.
- Managing stress effectively.
- Moderating alcohol consumption.
- Ensuring sufficient sleep (usually 7 to 9 hours) and addressing any sleep disorders.
- Quitting smoking.
- Following your healthcare provider’s advice on medication to manage risk factors for heart disease.
It’s crucial to acknowledge that certain risk factors, such as family history, age, and ethnicity, are beyond your control. Type 2 diabetes results from a mix of factors, emphasizing the condition’s complexity.
The prognosis for Diabetes
What is the long-term outlook for someone with diabetes?
The long-term outlook for diabetes depends on various factors, including the type of diabetes, the effectiveness and accessibility of diabetes management, the duration of diabetes, the presence of other health conditions, and the development of any diabetes-related complications. Unmanaged high blood sugar levels can lead to severe, often irreversible complications, reducing life expectancy and life quality. Diabetes ranks as the eighth leading cause of death in the United States, with heart attacks and strokes being common causes of death among those with diabetes.
Nonetheless, it’s possible to lead a healthy life with diabetes. Key factors that contribute to a more favourable prognosis include lifestyle modifications, regular physical activity, dietary adjustments, and consistent monitoring of blood sugar levels. Research indicates that maintaining A1c levels below 7% can significantly lower the risk of complications.
Living with Diabetes
When should you consult a healthcare professional? If you’re experiencing symptoms of diabetes, such as increased thirst and frequent urination, and haven’t been diagnosed, it’s important to seek medical advice. For those already diagnosed with diabetes, regular check-ups with a diabetes care specialist, like an endocrinologist, are crucial for effective management of the condition.
A message from Exaluh Solutions
Receiving a diabetes diagnosis is a significant turning point, but it doesn’t signify the end of a fulfilling and healthy life. Successfully managing diabetes requires ongoing attention and commitment. Although it may feel overwhelming initially, with time, you’ll become more adept at navigating the intricacies of the condition and understanding your body’s signals.
Regular visits to your healthcare provider(s) are essential. Managing diabetes is a collaborative effort, involving the support of medical professionals, as well as friends and family. Don’t hesitate to lean on them for assistance when needed.

