A stroke is a crisis. Understand the steps to take if you or someone close, to you is experiencing a stroke.

What exactly is a stroke?
A stroke is a condition that occurs when a part of the brain does not receive blood flow. This typically arises due to an obstructed artery or bleeding within the brain. When deprived of blood supply the brain cells in that region begin to perish due to lack of oxygen.
VITAL: A stroke is a life-threatening situation where time is of the essence. If you notice symptoms of a stroke in yourself or someone promptly seek assistance. The sooner treatment for the stroke begins the chances of recovery without life-threatening long-term disability.
Key indicators signalling an approaching stroke:
- Be alert for balance issues.
- Watch out for loss of vision, in one or both eyes and check if there’s double vision present.
- Request them to smile and observe any drooping on one or both sides of their face indicating muscle weakness or paralysis.
- Individuals experiencing a stroke often exhibit muscle weakness on one side; ask them to lift their arms up. If someone experiences a weakness, on one side (which was not present before) they may notice that one arm remains elevated while the other droops downward.
- When a person has a stroke, it can affect their ability to communicate effectively. They might experience slurred speech or difficulty in finding the words to express themselves.
- It is crucial to act in situations. If feasible check the time either on your wristwatch or a clock. Make note of when the symptoms appear. Providing this timing information to a healthcare professional can assist them in determining the treatment options for you.
Who is at risk of experiencing a stroke?
Strokes can happen to anyone regardless of age although certain individuals are more vulnerable than others. The likelihood of having a stroke increases with age (with two-thirds occurring in individuals aged 65 and older).
Several medical conditions elevate the risk of experiencing a stroke, such as blood pressure (hypertension), high cholesterol levels (hyperlipidemia), Type 2 diabetes and individuals with a history of stroke, heart attack or irregular heart rhythms like fibrillation.
How prevalent are strokes?
Strokes are widespread globally. Rank, as the leading cause of death worldwide.
In both the United States and Nigeria stroke ranks as the leading cause of death. Is increasingly becoming a significant concern. Strokes also stand out as a contributor, to disability.
How does a stroke impact the body?
Think of strokes affecting your brain in a way that heart attacks affect your heart. During a stroke, a section of your brain loses its blood supply depriving that area of oxygen. Without oxygen, the affected brain cells become starved. Fail to function, If brain cells remain deprived of oxygen for a longer period they will perish. When a sufficient number of brain cells die in an area the resulting damage becomes permanent leading to the loss of functions controlled by that region. However, restoring blood flow promptly can prevent damage or at least mitigate its impact. This underscores the importance of intervention when dealing with strokes.
What are the different types of strokes?
Strokes typically occur in two forms; Ischemic and Hemorrhagic.
Ischemic Stroke
Ischemia (pronounced as “iss key me uh”) arises when cells receive blood flow for oxygen supply. This usually occurs due to blockage, in brain blood vessels that obstruct blood circulation. Ischemic strokes are the type representing around 80% of all strokes.
They typically occur in a few ways:
- A clot forms in the brain (thrombosis).
- A clot fragment from elsewhere in the body breaks loose. It travels through the blood vessels until it lodges in the brain (embolism).
- Blockage of blood vessels (lacunar stroke) can occur due to high blood pressure, high cholesterol or Type 2 diabetes.
- Some strokes have no origins. These are referred to as cryptogenic strokes.
Hemorrhagic strokes
It involves bleeding in or around the brain. This can happen either within the brain tissue or in the subarachnoid space, the arachnoid membrane is where a thin spiderweb-like membrane surrounds the brain. The space, between your brain and it, is known as the space with “sub” meaning “under.” If blood vessels pass through and the arachnoid membrane is damaged, it can lead to a haemorrhage, which involves bleeding into the space and exerting pressure on the brain tissue below.
What are the symptoms and causes of strokes?
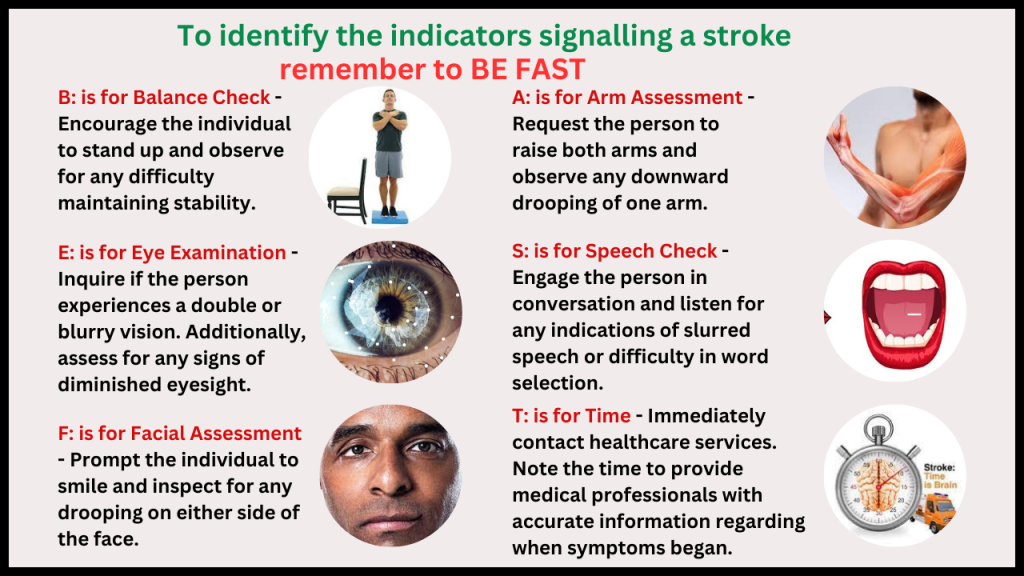
When it comes to strokes remembering BE FAST can be helpful; Balance, Eyes, Face droop, Arm weakness, Speech problems and Time. This mnemonic aids in recalling stroke symptoms related to balance issues, eye problems, facial drooping, arm weakness disparity speech difficulties while emphasizing the importance of treatment.
Stroke symptoms vary depending on which area of the brain is affected since different regions control functions. For instance, damage to the Brocas area in the brain impacts muscle use in the face and mouth, for speech. This explains why some individuals may experience slurred speech or have difficulty talking during a stroke episode.
The signs of stroke may include; weakness or paralysis, on one side difficulty speaking (aphasia) slurred speech (dysarthria) loss of muscle control on one side of the face sudden loss of one or more senses, blurry vision, coordination issues, dizziness, nausea, neck stiffness, emotional changes, confusion, seizures, memory problems, severe headaches, fainting spells, coma and transient ischemic attack (TIA).
A transient ischemic attack (TIA) is similar to a stroke. With effects. It serves as a warning sign, for a risk of a stroke and requires immediate medical attention.
Strokes can be caused by blood clots leading to strokes or haemorrhages causing strokes. Strokes can occur due to a variety of factors like Atherosclerosis clotting disorders and atrial fibrillation linked to sleep apnea. Heart abnormalities such as defect or ventricular septal defect as well as microvascular ischemic disease that blocks tiny blood vessels in the brain can also contribute to their onset. Additionally, hemorrhagic strokes may be caused by prolonged blood pressure levels, brain aneurysms, tumors, in the brain (including cancer) and conditions that affect blood vessel health like moyamoya disease.
Related conditions
Several other conditions and factors can contribute to a person’s stroke risk. These include:
- Alcohol use disorder.
- High blood pressure (this can play a role in all types of strokes, not just hemorrhagic ones because it can contribute to blood vessel damage that makes a stroke more likely).
- High cholesterol (hyperlipidemia).
- Migraine headaches (they can have symptoms similar to a stroke, and people with migraines — especially migraines with auras — also have a higher risk of stroke at some point in their life).
- Type 2 diabetes.
- Smoking and other forms of tobacco use (including vaping and smokeless tobacco).
- Drug misuse (including prescription and non-prescription drugs).
Is Stroke contagious?
Strokes are not contagious and you can’t pass them to or get them from other people.
Diagnosis and Tests
How are strokes diagnosed?
A healthcare provider can diagnose a stroke using a combination of a neurological examination, diagnostic imaging and other tests. During a neurological examination, a provider will have you do certain tasks or answer questions. As you perform these tasks or answer these questions, the provider will look for telltale signs that show a problem with how part of your brain works.
What tests will be done to diagnose this condition?
The most common tests that happen when a healthcare provider suspects a stroke include:
- Computerized tomography (CT) scan.
- Lab blood tests (looking for signs of infections or heart damage, checking clotting ability and blood sugar levels, testing how well kidneys and liver function, etc.).
- Electrocardiogram (abbreviated ECG or EKG) to make sure that a heart issue isn’t the source of the problem.
- Magnetic resonance imaging (MRI) scans.
- Electroencephalogram (EEG), though less common, can rule out seizures or related problems.
Management and Treatment of Strokes
How are strokes treated?
Treating a stroke depends on many different factors. The most important factor in determining treatment is what kind of stroke a person has.
Ischemic: With ischemic strokes, the top priority is restoring circulation to affected brain areas. If this happens fast enough, it’s sometimes possible to prevent permanent damage or at least limit a stroke’s severity. Restoring circulation usually involves a certain medication type called thrombolytics, but may also involve a catheterization procedure.
Hemorrhagic: With hemorrhagic strokes, treatment depends on the location and severity of the bleeding. Reducing blood pressure is often the top priority because this will reduce the amount of bleeding and keep it from getting worse. Another treatment option is to improve clotting so the bleeding will stop. Surgery is sometimes necessary to relieve pressure on your brain from accumulated blood.
What medications or treatments are used for Strokes?
The medications and treatments used vary depending on the type of stroke and how soon a person receives treatment after the stroke. There are also long-term treatments for stroke. These happen in the days and months after emergency treatment deals with a stroke’s immediate threat.
Overall, your healthcare provider is the best person to tell you what kind of treatment(s) they recommend. They can tailor the information they provide to your specific case, including your medical history, personal circumstances and more.
Some examples of treatments for stroke are as follows:
For Ischemic stroke: Thrombolytic drugs (within three to four and a half hours), Thrombectomy (within 24 hours if there’s no significant brain damage), Blood pressure management.
For Hemorrhagic stroke: Blood pressure management, Reversal of any medication that might increase bleeding, use of medications or surgery to reduce pressure inside your skull.
Thrombolytic drugs
Thrombolytic drugs (their name is a combination of the Greek words “thrombus,” which means “clot,” and “lysis,” which means “loosening/dissolving”) are an option within the first three hours after stroke symptoms start. These medications dissolve existing clots. But they’re only an option within that three- to four-and-a-half-hour time frame because, after that, they increase the risk of dangerous bleeding complications.
Mechanical thrombectomy
In some cases, especially ones where thrombolytic drugs aren’t an option, a catheterization procedure known as mechanical thrombectomy is an option. Thrombectomy procedures are also time-sensitive, and the best window for these procedures is within 24 hours after symptoms start. This procedure involves inserting a catheter (tube-like) device into a major blood vessel and steering it up to the clot in your brain. Once there, the catheter has a tool at its tip that can remove the clot.
Blood pressure management
Because high blood pressure is usually why hemorrhagic strokes happen, lowering blood pressure is a key part of treating them. Lowering blood pressure limits bleeding and makes it easier for clotting to seal the damaged blood vessel.
Clotting support
Your body’s clotting ability relies on a process called hemostasis to stop bleeding and repair injuries. Supporting hemostasis involves the infusion of medications or blood factors that make it easier for clotting to happen. Examples include vitamin K therapy, prothrombin or clotting factor infusions, and more. This treatment is most common with hemorrhagic strokes and can help control bleeding (especially for people who take blood-thinning medications).
Surgery
In some cases, surgery is necessary to relieve the pressure on your brain. This is especially true with subarachnoid hemorrhages, which are easier to reach because they’re on the outer surface of your brain.
Supportive treatments for Strokes and other methods
There are several other ways that stroke treatment can happen. Some of these treatments are supportive directly, while others help avoid complications. Your healthcare provider can tell you more about these other treatments and which ones they recommend and why.
Stroke rehabilitation
One of the most important ways to treat stroke is to help a person recover or adapt to the changes in their brain. That’s especially true when it comes to helping them regain abilities they had before the stroke. Stroke rehabilitation is a major part of recovery for most people who have a stroke. That rehabilitation can take many forms, including:
Speech therapy: This can help you regain language and speaking abilities and improve your ability to control muscles that help you breathe, eat, drink and swallow.
Physical therapy: This can help you improve or regain the ability to use your hands, arms, feet and legs. This can also help with balance issues, muscle weakness and more.
Occupational therapy: This can help retrain your brain so you can go about your activities of daily life. This therapy is beneficial in improving precise hand movements and muscle control.
Cognitive therapy: This can be helpful if you’re having memory problems. It can also help if you have difficulty with activities that require focus or concentration that you can do before.
Other therapies are possible, depending on your case and circumstances. Your healthcare provider is the best person to tell you what kind of treatments can benefit you.
Complications/side effects of the treatment
The side effects of stroke treatments depend greatly on the type of stroke, the treatments used, your medical history and more. Your healthcare provider can tell you more about the side effects you can or should expect and what you can do to manage or even prevent them.
How can I take care of myself or manage the symptoms?
A stroke is a life-threatening medical emergency, and you shouldn’t try to self-diagnose or self-treat it. If you or someone with you has stroke symptoms, you should immediately seek medical assistance. The longer it takes for stroke treatment to begin, the greater the risk of permanent brain damage or death.
How soon after treatment will I feel better?
The recovery time and how long it takes to feel better after treatment both depend on many factors. Your healthcare provider is the best person to tell you what you can expect and the likely timeline for your recovery.
Prevention of Strokes
How can I reduce my risk of having a stroke or prevent it entirely?
There are many things you can do to reduce your risk of having a stroke. While this doesn’t mean you can prevent a stroke, it can lower your risk. Actions you can take include:
Improve your lifestyle. Eating a healthy diet and adding exercise to your daily routine can improve your health. You should also make sure to get enough sleep (the recommended amount is seven to eight hours).
Avoid risky lifestyle choices or make changes to your behaviours. Smoking and tobacco use, including vaping, recreational drug use or prescription drug misuse, and alcohol misuse can all increase your risk of having a stroke. It’s important to stop these or never start them. If you struggle with any of these, talking to your healthcare provider is important. Your provider can offer you guidance and resources that can help you change your lifestyle to avoid these behaviours.
Manage your health conditions and risk factors. There are several conditions, such as obesity, abnormal heart rhythms, sleep apnea, high blood pressure, Type 2 diabetes or high cholesterol, which can increase your risk of having an ischemic stroke. If you have one or more of these conditions, you must do what you can to manage them, especially by taking medications — such as blood thinners — as prescribed by your provider. Doing that earlier in life can you avoid severe stroke-related problems later in life.
See your healthcare provider for a checkup or wellness visit annually. Yearly wellness visits can detect health problems — especially ones that contribute to having a stroke — long before you feel any symptoms.
Is there anything I shouldn’t eat or drink with this condition?
If you’re at risk for any kind of stroke, your healthcare provider may recommend changing your diet to avoid increases in blood pressure. Examples of this include:
- Beverages that contain caffeine, such as coffee, tea, soft drinks, etc.
- Foods that contain a lot of salt or sodium, which can increase blood pressure.
- Foods that are high in saturated fats, such as fried foods, etc.
- Alcohol or recreational stimulant drugs (cocaine, amphetamines/methamphetamine, etc.).
Outlook / Prognosis
What can I expect if I have this condition?
If you have a stroke, many factors affect what you can expect, such as how big it is and where it is in your brain. There are also some key differences between ischemic and hemorrhagic strokes.
Ischemic strokes: In general, the more severe an ischemic stroke is, the worse the damage. When brain damage is more severe, it’s more likely that you’ll lose certain abilities, at least temporarily. The faster you get medical attention for stroke symptoms, the better your chances that these effects are temporary or less severe.
Hemorrhagic stroke: These strokes usually cause much worse symptoms, especially when bleeding is more severe. The symptoms of hemorrhagic stroke tend to get worse quickly. People with hemorrhagic strokes tend to cause severe headaches, seizures and coma.
How long does a stroke last?
A stroke lasts as long as there’s a lack of blood flow to part of your brain. Without treatment, a stroke will continue until the brain cells in the affected areas of your brain die, causing permanent damage.
Even after you receive treatment for a stroke, it’s common for the effects to linger. Most people will take weeks or even months to recover. Most of the progress in recovery happens within the first six months to 18 months (approximately) after a stroke. Further progress is possible after that, but can be harder to achieve or take longer.
When can I go back to work or school?
Your healthcare provider is the best person to tell you when you can return to your usual routine and activities. But it’s important not to push yourself too hard. Without enough time to recover, you could have another stroke or other complications.
What’s the outlook for this condition?
Strokes have the potential to cause death when they’re severe or if they go too long without treatment. However, the outlook can still vary widely depending on many factors. Those factors include where in your brain a stroke happens, how severe it is, your health history and more.
Your healthcare provider is the best person to tell you more about the outlook for your situation. The information they provide will be the most accurate and relevant information that you can get.
Living with Stroke
How do I take care of myself?
If you have a stroke, your healthcare provider will talk with you about a plan for treatment and the timeline for your recovery. They may also prescribe medications, recommend therapy options and more. It’s important to talk with your healthcare provider about why they recommend these and what they can do for you.
Once you and your provider finalize the treatment plan, you must follow it as closely as possible. Doing that will give you the best chance to maximize how much you recover. Other things you can do include:
Take your medication. Medications that you take after a stroke can prevent having another.
Go to rehabilitation/therapy appointments. These appointments are critical to your recovery. Going to these appointments and putting in your best effort can make a big difference in how much you recover from a stroke.
Take care of your mental health. Depression and anxiety are prevalent after having a stroke. Experiencing these doesn’t mean you’re weak or hopeless, but letting them go untreated can make it harder for you to recover. Talk to your healthcare provider about these feelings if you have them. They can recommend care that can help keep mental health concerns from standing in the way of your recovery.
Make recommended lifestyle changes as best you can. Health concerns like your blood pressure, blood sugar and cholesterol can all play a role in your recovery from a stroke. Managing these can also help you avoid another stroke in the future. If you use tobacco products (including vaping products) of any kind, quitting them can also help greatly.
When should I see my healthcare provider?
You should see your healthcare provider as recommended. You should also see them if you notice any new symptoms affecting you, especially symptoms that might have a connection to your previous stroke. Even symptoms that don’t seem connected might be important, so don’t wait to discuss them with your healthcare provider.
When should I go to the ER?
You should call your healthcare provider and go to the nearest ER if you experience any symptoms of another stroke (see the FAST criteria at the top of this article to know the symptoms for which you should watch).
You should also go to the hospital if you experience any of the symptoms of dangerous complications that are common after a stroke. The most common complicating conditions include:
- Pneumonia.
- Deep vein thrombosis (DVT).
- Pulmonary embolism.
- Heart attack.
- Seizures.
Word of Advice from Exaluh Solutions
A stroke is your brain’s version of a heart attack, making it a critical, life-threatening medical emergency. Strokes are also time-sensitive, and delays in care can lead to permanent brain damage and death. Strokes can be frightening for those who experience them or people nearby.
However, the treatment options for stroke are expanding every day thanks to advances in our understanding of the brain, technological leaps in imaging and new medications. If you notice the symptoms of a stroke in yourself or someone you’re with immediate medical attention is critical. The faster a person having a stroke gets medical care, the more likely the effects of the stroke will be limited or even reversible.

